3D Laparoscopic Pyeloplasty
Indications, Procedure, Advantages, Recovery and Support
What is 3D Laparoscopic Pyeloplasty?
3D Laparoscopic Pyeloplasty is a minimally invasive surgical technique used to correct ureteropelvic junction obstruction (UPJ), a condition where the flow of urine from the kidney to the ureter is blocked or restricted. This procedure involves reconstructing the affected area to restore normal urine flow, preventing further complications such as pain, kidney infections, and possible kidney damage.
Using advanced 3D laparoscopy, surgeons gain enhanced depth perception and precision during the procedure. Small incisions are made to insert laparoscopic instruments and a 3D camera, allowing the surgeon to remove the narrowed segment and reconnect the healthy parts of the kidney and ureter. This 3D technology aids in improving the accuracy and control of the surgeon's movements, reducing tissue damage and minimizing bleeding.
The advantages of 3D laparoscopic pyeloplasty over traditional open surgery include smaller incisions, less postoperative pain, faster recovery, and minimal scarring. This procedure is particularly suited for patients who experience persistent symptoms from UPJ obstruction, such as flank pain, recurrent kidney infections, or hydronephrosis (swelling of the kidney due to urine buildup).
In preparation for the procedure, patients undergo a comprehensive evaluation, including imaging tests like CT scans or MRIs, to assess the severity of the obstruction. The recovery process is generally shorter than traditional open surgery, with most patients resuming light activities within a few weeks. 3D Laparoscopic Pyeloplasty offers an effective and less invasive solution for UPJ obstruction, enhancing quality of life and preserving kidney health.
Indications for 3D Laparoscopic Pyeloplasty
Indications for 3D Laparoscopic Pyeloplasty focus on addressing ureteropelvic junction obstruction (UPJ), where the passage of urine from the kidney to the ureter is blocked or narrowed. This condition can lead to kidney damage if left untreated, making pyeloplasty a crucial intervention for many patients. Here are some primary indications:
1. Symptomatic UPJ Obstruction
- Persistent Pain: Patients with chronic flank pain or discomfort, typically aggravated by fluid intake, often benefit from surgical intervention to relieve obstruction.
- Recurrent Urinary Tract Infections (UTIs): Frequent UTIs linked to urine stasis at the UPJ indicate the need for pyeloplasty to prevent further infections and complications.
2. Hydronephrosis
- Progressive Kidney Swelling: Hydronephrosis, caused by a build-up of urine due to obstruction, can lead to kidney tissue damage over time. Surgical correction is often recommended to restore normal urine flow and reduce swelling.
- Impaired Kidney Function: When obstruction affects kidney function, 3D laparoscopic pyeloplasty helps restore kidney health and prevent permanent damage.
3. Deteriorating Kidney Function
- Reduced Kidney Filtration: In cases where obstruction leads to decreased renal filtration, pyeloplasty becomes necessary to maintain kidney function and prevent chronic kidney disease.
- Renal Scan Results: Imaging studies that reveal reduced function or differential function between the kidneys are strong indicators for surgical intervention.
4. Congenital UPJ Obstruction
- Children and Young Adults: Many patients with UPJ obstruction are diagnosed early in life. While some cases resolve naturally, symptomatic cases or those with significant kidney function impairment often require intervention.
- Delayed Diagnosis: Some congenital cases are not diagnosed until adulthood. When symptoms appear later in life, laparoscopic pyeloplasty is often preferred for its minimally invasive approach.
5. Failed Prior Treatments or Recurrence
- Previous Failed Surgeries: Some patients may have undergone an initial surgery that was unsuccessful in resolving the UPJ obstruction. 3D laparoscopic pyeloplasty offers an effective alternative for these complex cases.
- Recurrent Obstruction: In cases where an obstruction has redeveloped, 3D laparoscopic pyeloplasty provides an advanced and precise option to address the recurring issue.
6. Prevention of Further Complications
- Kidney Stones: UPJ obstruction can lead to kidney stones due to urine stasis. By improving urine flow, pyeloplasty helps reduce the risk of stone formation.
- Chronic Inflammation: Persistent inflammation due to UPJ obstruction may lead to scarring and further damage. Surgical intervention helps minimize this risk.
3D laparoscopic pyeloplasty provides an effective, minimally invasive solution for managing UPJ obstruction, preserving kidney function, and improving the patient’s quality of life. It’s especially suited for patients requiring precise correction with faster recovery and reduced postoperative discomfort.
Procedure and Preparation for 3D Laparoscopic Pyeloplasty
Procedure and Preparation for 3D Laparoscopic Pyeloplasty involve careful planning and specialized surgical techniques designed to treat ureteropelvic junction (UPJ) obstruction. Here’s a step-by-step overview, covering both the preparation and surgical process.
Preparation for 3D Laparoscopic Pyeloplasty
1. Preoperative Evaluation
- Medical History and Physical Exam: The surgeon will review the patient's medical history, including any previous kidney or urinary tract issues, and perform a comprehensive physical examination.
- Imaging Studies: Detailed imaging tests, such as CT scans, MRIs, and renal ultrasounds, help to confirm the diagnosis of UPJ obstruction, assess the kidney’s condition, and determine the precise location and severity of the blockage.
- Renal Function Tests: Blood tests, including serum creatinine levels and other renal function indicators, provide baseline information about kidney function, essential for planning the procedure.
- Nuclear Renal Scan: This scan measures how well each kidney is functioning and can highlight any significant disparities, helping the surgeon decide on the optimal approach.
2. Preoperative Instructions
- Medication Adjustments: Patients may need to stop blood-thinning medications, such as aspirin or other anticoagulants, to reduce the risk of bleeding during surgery.
- Fasting: Fasting is typically required for 8-12 hours before surgery to prepare for general anesthesia, reducing the risk of aspiration.
- Hydration and Electrolyte Balance: Preoperative hydration is managed to ensure patients are well-hydrated while avoiding over-hydration. Some may also receive a saline IV to ensure electrolyte balance during surgery.
3. Anesthesia Planning
- General Anesthesia Consultation: A consultation with the anesthesiologist helps ensure patients are aware of anesthesia protocols, understand the sedation process, and have a chance to ask questions.
Procedure for 3D Laparoscopic Pyeloplasty
1. Anesthesia and Positioning
- The patient is placed under general anesthesia and positioned on the operating table in a lateral or semi-lateral position, depending on the surgeon’s preference and the specific anatomy involved.
2. Trocar Placement and Instrument Setup
- 3D Laparoscopic Camera Insertion: Small incisions (usually three to five) are made to allow insertion of trocars, through which the laparoscopic instruments and a 3D camera are introduced. The 3D camera provides a high-definition, three-dimensional view of the surgical area, enhancing depth perception and precision.
- Instrument Insertion: Specialized laparoscopic instruments are inserted through the trocars, and the surgeon adjusts their positioning to optimize access to the kidney and ureter.
3. Isolation and Dissection of the Ureter and Renal Pelvis
- The surgeon carefully isolates the UPJ area by dissecting around the obstructed segment. This step requires precision to avoid damage to surrounding blood vessels and tissues.
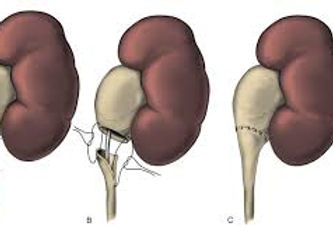
- Removal of Obstructed Segment: Once isolated, the surgeon removes the narrowed section of the ureter where the obstruction is located, creating a clear path for urine flow.
4. Reconnection and Reconstruction (Anastomosis)
- Reconnection of Ureter and Renal Pelvis: The healthy end of the ureter is carefully reattached to the renal pelvis using fine sutures. The 3D visualization allows for optimal precision in aligning the structures, reducing the risk of leakage or recurrence of obstruction.
- Insertion of Ureteral Stent: A temporary stent is placed within the ureter to support healing, ensure the passage remains open, and facilitate urine flow from the kidney to the bladder while the tissues heal. This stent is typically removed a few weeks after surgery.
5. Closure and Final Inspection
- The surgical area is carefully inspected to ensure no bleeding or leaks. The instruments and camera are removed, and the small incisions are closed with sutures or surgical glue.
- Sterile Dressings: Sterile dressings are applied to the incision sites, helping to prevent infection and promote healing.
Postoperative Recovery and Care
1. Initial Recovery
- Patients are monitored closely for any immediate postoperative complications, such as bleeding or infection, and may remain in the hospital for 1-2 days for observation.
2. Pain Management and Antibiotics
- Pain is typically managed with mild analgesics, as laparoscopic procedures generally cause less discomfort compared to open surgery. Antibiotics are administered to prevent infection.
3. Stent Removal
- The ureteral stent is usually removed 4-6 weeks postoperatively in a quick outpatient procedure, after the healing is confirmed through follow-up imaging.
4. Follow-Up Appointments
- Follow-up appointments are essential to assess the surgical outcome and kidney function. Imaging may be repeated to confirm the success of the procedure and ensure no recurring blockage or complications.
3D laparoscopic pyeloplasty offers a highly effective, minimally invasive approach to treating UPJ obstruction, with faster recovery, less postoperative pain, and improved outcomes due to the precision and accuracy provided by 3D imaging.
Advantages and Risks of 3D Laparoscopic Pyeloplasty
Advantages and Risks of 3D Laparoscopic Pyeloplasty are essential to consider when evaluating this advanced procedure as a treatment for ureteropelvic junction (UPJ) obstruction. This minimally invasive surgery offers numerous benefits over traditional open surgery, but like any procedure, it also carries potential risks.
Advantages of 3D Laparoscopic Pyeloplasty
1. Enhanced Precision and Visualization
- 3D Imaging: The 3D laparoscopic approach offers high-definition, three-dimensional visualization, providing surgeons with better depth perception and clarity of anatomical structures.
- Accurate Suturing: The improved visualization allows for precise suturing during the reconstruction of the ureter and renal pelvis, reducing the risk of leaks or improper alignment.
2. Minimally Invasive Approach
- Smaller Incisions: This technique uses small incisions, minimizing tissue disruption compared to open surgery.
- Less Scarring: Smaller incisions lead to less noticeable scars, enhancing cosmetic outcomes.
3. Reduced Postoperative Pain
- Lower Pain Levels: Patients often experience less postoperative pain due to the smaller incisions and reduced tissue handling. This typically results in a decreased need for strong pain medications.
- Quicker Recovery: The minimally invasive approach supports faster recovery, allowing patients to return to normal activities sooner.
4. Shorter Hospital Stay
- Faster Discharge: Most patients require only 1-2 days of hospitalization, reducing the risk of hospital-acquired infections and promoting a quicker return to home.
5. Reduced Risk of Complications
- Lower Risk of Infection: Smaller incisions and a shorter hospital stay minimize exposure to potential infections.
- Controlled Bleeding: With precise control during the procedure, there is generally less blood loss, reducing the need for blood transfusions.
6. Higher Success Rates
- Durable Results: Studies have shown high success rates for pyeloplasty procedures performed laparoscopically, with lasting improvements in kidney function and urine flow.
- Lower Recurrence of Obstruction: The accurate removal of the obstructed segment and effective reconnection help reduce the likelihood of re-obstruction.
Risks of 3D Laparoscopic Pyeloplasty
1. Potential for Surgical Complications
- Infection: Despite the minimally invasive nature, there is still a small risk of infection at the incision sites or within the urinary tract. Antibiotics are typically administered to reduce this risk.
- Bleeding: Although less common, there is a risk of bleeding, especially if nearby blood vessels are inadvertently damaged. This may require additional interventions or a blood transfusion in rare cases.
2. Risk of Urinary Leak
- Anastomotic Leak: Leaks can occasionally occur at the site where the ureter is reconnected to the renal pelvis. This may necessitate a longer recovery period, additional procedures, or stent placement to aid healing.
3. Ureteral Stent-Related Discomfort
- Temporary Stent Side Effects: The stent placed to aid healing can cause temporary discomfort, frequent urination, or bladder irritation. These symptoms typically subside once the stent is removed after a few weeks.
4. Possible Re-obstruction
- Recurrence of UPJ Obstruction: In rare cases, scar tissue or improper healing can lead to re-narrowing of the ureter, necessitating additional interventions to correct the blockage.
5. Anesthetic Risks
- General Anesthesia: The procedure requires general anesthesia, which carries its own set of risks, especially for patients with pre-existing health conditions. Common risks include reactions to medications, respiratory issues, or postoperative nausea.
6. Longer Operative Time
- Slightly Extended Surgery Duration: 3D laparoscopic procedures can take longer than open surgeries due to the setup and precise technique. While not typically a major issue, longer operative time can occasionally lead to increased anesthesia risks or fatigue.
3D laparoscopic pyeloplasty offers a highly effective, minimally invasive solution for UPJ obstruction with significant benefits, such as reduced pain, faster recovery, and precise results. While the risks are relatively low, it’s important for patients to have a thorough preoperative discussion with their surgeon to understand both the benefits and potential complications associated with the procedure.
Postoperative Care and Recovery after 3D Laparoscopic Pyeloplasty
Postoperative Care and Recovery after 3D Laparoscopic Pyeloplasty are essential to ensure a successful outcome, minimize complications, and support a quick return to daily activities. Here is an in-depth look at the steps involved in postoperative care and what patients can expect during recovery.
1. Immediate Postoperative Care
- Hospital Stay: Most patients stay in the hospital for 1-2 days following the procedure to allow medical staff to monitor their initial recovery, manage pain, and address any immediate postoperative needs.
- Pain Management: Due to the minimally invasive nature of the procedure, postoperative pain is usually mild and manageable. Patients are typically prescribed over-the-counter pain relievers or mild analgesics. Stronger pain medications are rarely needed.
- **Hydration and Nutrition**: Patients may be given fluids intravenously immediately after the procedure. Oral intake is gradually reintroduced, starting with clear liquids and advancing to a regular diet as tolerated.
2. Monitoring and Follow-Up Tests
- Vital Signs and Urine Output: In the early stages of recovery, nurses and healthcare providers monitor vital signs and urine output to ensure the kidneys are functioning properly and there are no signs of complications.
- Blood and Urine Tests: Routine tests may be performed to check for signs of infection, kidney function, and hydration levels. These tests provide baseline data to monitor the patient's progress throughout recovery.
- Imaging Studies: In some cases, an ultrasound or CT scan may be done postoperatively to verify the success of the procedure, ensuring there is no urine leakage or any signs of obstruction recurrence.
3. Managing the Ureteral Stent
- Purpose of the Stent: A temporary ureteral stent is usually placed during surgery to keep the newly reconstructed ureter open and to allow urine to flow smoothly from the kidney to the bladder while the tissues heal.
- Stent-Related Symptoms: The stent may cause mild discomfort, frequent urination, or a sensation of urgency. These symptoms are generally temporary and should subside once the stent is removed.
- Stent Removal: The stent is typically removed 4-6 weeks after surgery in a brief outpatient procedure. Removal is straightforward, with most patients experiencing minimal discomfort during the process.
4. Incision Care and Activity Restrictions
- Incision Care: Small incisions from the laparoscopic procedure should be kept clean and dry to prevent infection. Patients are usually advised to avoid soaking the incisions in water (e.g., baths or swimming) until the incisions are fully healed, which generally takes about 1-2 weeks.
- Dressings: Surgical dressings are generally removed within a few days. Afterward, patients may be instructed to use band-aids or leave the incisions uncovered if healing progresses well.
- Activity Restrictions: Patients are encouraged to walk gently and resume light activity as soon as possible to prevent blood clots and promote circulation. However, they should avoid heavy lifting, strenuous activities, and twisting movements for at least 4-6 weeks to protect the surgical site.
5. Diet and Hydration
- Balanced Diet: A balanced diet rich in fruits, vegetables, lean proteins, and whole grains supports the healing process. It’s also essential for maintaining kidney function.
- Hydration: Staying well-hydrated is crucial, as water helps flush the kidneys and supports healing. Patients are typically advised to drink plenty of water and avoid excess caffeine or alcohol, which can strain the kidneys.
6. Follow-Up Appointments
- Scheduled Check-Ups: Regular follow-up appointments are essential to monitor recovery. During these visits, the surgeon will evaluate the healing process, review any symptoms, and confirm that kidney function has returned to normal.
- Imaging Tests: Follow-up imaging, such as ultrasound or CT scans, may be performed a few weeks or months after surgery to ensure there is no recurrence of the obstruction or other complications.
- Blood and Urine Tests: These tests will continue to monitor renal function and check for signs of infection, ensuring that the procedure has been successful and that the kidney is functioning as expected.
7. Recognizing Signs of Complications
Patients should be aware of and report any unusual symptoms to their healthcare provider immediately. These may include:
- Fever or Chills: Could indicate an infection.
- Severe Pain: Beyond what is expected or not relieved by prescribed medications.
- Blood in Urine: A small amount of blood in urine may be normal initially, but persistent or heavy bleeding could indicate a problem.
- Difficulty Urinating or Reduced Urine Output: Could suggest an issue with the stent or obstruction.
8. Long-Term Recovery and Lifestyle Adjustments
- Gradual Return to Normal Activities: Most patients can return to normal activities within 2-4 weeks, with full recovery expected around the 6-week mark. Physical activities should be resumed gradually and with the guidance of a healthcare provider.
- Preventive Measures for Kidney Health: A healthy lifestyle, including a balanced diet, regular exercise, and adequate hydration, supports kidney health and helps prevent future issues.
- Avoiding High-Sodium and Processed Foods: Limiting sodium intake can reduce the risk of high blood pressure and strain on the kidneys, supporting overall kidney health.
3D Laparoscopic Pyeloplasty offers a quicker and less painful recovery compared to traditional open surgery. With careful postoperative care and adherence to medical guidelines, patients can expect excellent outcomes, restored urine flow, and a return to daily life with minimal disruption.
Why Choose Dr. Marinos Vasilas for 3D Laparoscopic Pyeloplasty
Choosing Dr. Marinos Vasilas for your 3D laparoscopic pyeloplasty ensures expert care and advanced surgical techniques.
Expertise in 3D Laparoscopic Surgery
Dr. Vasilas specializes in 3D laparoscopic procedures, offering enhanced depth perception and precision during surgery. This expertise leads to improved outcomes and faster recovery times for patients.
Collaborations with Leading Clinics
He collaborates with top-tier clinics, including "Lefkos Stavros" in Athens and "Euromedica" in Rhodes, both equipped with state-of-the-art facilities. These partnerships ensure comprehensive care and access to the latest medical technologies.
Personalized Patient Care
Dr. Vasilas emphasizes a patient-centered approach, providing individualized support from initial consultation through postoperative recovery. His commitment to transparency and empathy fosters a trusting doctor-patient relationship.
Advanced Surgical Techniques
Utilizing 3D laparoscopic technology, Dr. Vasilas performs surgeries with minimal invasiveness, reducing postoperative pain and accelerating healing. This approach benefits patients by minimizing hospital stays and promoting quicker returns to daily activities.
By choosing Dr. Marinos Vasilas for your 3D laparoscopic pyeloplasty, you are opting for a surgeon with specialized skills, access to premier medical facilities, and a dedication to personalized, compassionate care.
Frequently Asked Questions (FAQ) for 3D Laparoscopic Pyeloplasty
1. What is 3D Laparoscopic Pyeloplasty?
- Answer: 3D Laparoscopic Pyeloplasty is a minimally invasive procedure used to correct ureteropelvic junction (UPJ) obstruction, where the flow of urine from the kidney to the ureter is restricted. This approach uses 3D imaging for enhanced precision, allowing surgeons to reconstruct the blocked area of the ureter and restore normal urine flow.
2. Why choose 3D laparoscopic over traditional open surgery?
- Answer: The 3D laparoscopic approach offers several advantages over open surgery, including smaller incisions, reduced pain, faster recovery times, and minimal scarring. The 3D visualization also enhances the surgeon's accuracy, leading to better outcomes with fewer risks of complications.
3. What causes UPJ obstruction, and how is it diagnosed?
- Answer: UPJ obstruction can be congenital (present from birth) or acquired due to scarring, previous surgery, or kidney stones. Diagnosis typically involves imaging tests, such as an ultrasound, CT scan, or MRI, to assess the blockage and kidney function.
4. What are the preparation steps before 3D laparoscopic pyeloplasty?
- Answer: Preparation includes a full medical evaluation, imaging tests to confirm UPJ obstruction, and renal function tests to assess the kidney’s health. Patients may need to adjust medications and follow fasting instructions the night before surgery.
5. How long does the procedure take?
- Answer: The surgery generally takes 2-3 hours, but this may vary based on the severity of the obstruction and the patient’s anatomy. The 3D laparoscopic approach is precise but can require more time than traditional methods.
6. What should I expect during recovery?
- Answer: Most patients can expect a short hospital stay of 1-2 days. Initial recovery includes mild discomfort managed by pain medication, and most patients can resume light activities within 1-2 weeks. Full recovery is typically expected in 4-6 weeks.
7. Is a stent placed during the surgery, and how long does it stay?
- Answer: Yes, a temporary ureteral stent is usually placed to keep the surgical area open and aid healing. It typically remains in place for 4-6 weeks post-surgery and is removed in a brief outpatient procedure.
8. What are the potential risks of 3D Laparoscopic Pyeloplasty?
- Answer: Although the risks are lower with laparoscopic surgery, potential complications include infection, bleeding, urinary leaks, or rare recurrence of obstruction. Careful surgical technique and postoperative follow-up help to minimize these risks.
9. When can I return to work or normal activities?
- Answer: Most patients with desk jobs or light physical demands can return to work within 2-3 weeks. Those with more physically demanding jobs may need to wait 4-6 weeks. Strenuous activity, heavy lifting, and vigorous exercise should be avoided until fully cleared by your surgeon.
10. What lifestyle changes are recommended after pyeloplasty?
- Answer: Patients are advised to maintain a healthy diet, stay hydrated, and avoid high-sodium or processed foods to support kidney health. Regular follow-up appointments are essential to monitor kidney function, particularly in the first year post-surgery.
11. How successful is 3D Laparoscopic Pyeloplasty in treating UPJ obstruction?
- Answer: This procedure has a high success rate, with most patients experiencing relief from symptoms and improved kidney function. The 3D approach enhances surgical precision, which supports long-lasting results and reduces the likelihood of recurrence.
These FAQs cover key aspects of 3D Laparoscopic Pyeloplasty, helping patients understand what to expect, the benefits, potential risks, and how best to prepare for and recover from the procedure. For any additional questions, consulting directly with a specialist like Dr. Marinos Vasilas can provide tailored information.
Contact Us for 3D Laparoscopic Pyeloplasty
If you need more information on 3D laparoscopic pyeloplasty or wish to schedule an appointment with Dr. Marinos Vasilas, our team is here to assist you. Contact us to receive specialized advice and complete guidance through every stage of the process, from preparation to recovery.
- Phone: +302241031123
- Email: marinosvasilas@gmail.com
- Location and Map:
- Athens – "Lefkos Stavros" Clinic
- Rhodes – "Euromedica" Clinic
Please feel free to reach out to discuss your needs and find personalized treatment solutions.
